What is Pneumonia?
Infection that inflames air sacs in one or both lungs, which may fill with fluid.
With pneumonia, the air sacs may fill with fluid or pus. The infection can be life-threatening to anyone, but particularly to infants, children and people over 65.
Epidemiology of Pneumonia.
The estimated worldwide incidence of community-acquired pneumonia varies between 1.5 to 14 cases per 1000 person-years, and this is affected by geography, season, and population characteristics. In the United States, the annual incidence is 24.8 cases per 10,000 adults with higher rates as age increases.
What causes Pneumonia?
Common Causes of Pneumonia are viruses, bacteria, and fungi can all cause pneumonia. In the United States, common causes of viral pneumonia are influenza, respiratory syncytial virus (RSV), and SARS-CoV-2 (the virus that causes COVID-19). A common cause of bacterial pneumonia is Streptococcus pneumoniae (pneumococcus).
- Cough, which may produce greenish, yellow or even bloody mucus.
- Fever, sweating and shaking chills.
- Shortness of breath.
- Rapid, shallow breathing.
- Sharp or stabbing chest pain that gets worse when you breathe deeply or cough.
- Loss of appetite, low energy, and fatigue.
Stages of Pneumonia
The four stages of lobar pneumonia include:
Stage 1: Congestion
During the congestion phase, the lungs become very heavy and congested due to infectious fluid that has accumulated in the air sacs. During this stage, your older loved one may experience early pneumonia symptoms such as:- Coughing
- A feeling of heaviness in the chest
- Loss of appetite
- Fatigue
- Rapid breathing
Stage 2: Red hepatization
Red blood cells and immune cells that enter the fluid-filled lungs to combat the infection give the lungs a red appearance. Although the body is beginning to fight the infection during this stage, your loved one may experience worsening symptoms such as:- Increasingly productive cough
- Shortness of breath
- Muscle aches
- Headache
- Extreme fatigue
- Fever
- Chills
- Sweating
- Blue lips or fingernails due to low levels of oxygen in the blood.
Some older adults may experience confusion or delirium during this stage. If your senior loved one experiences severe symptoms such as difficulty breathing, high fever, or blue lips or fingernails, you should seek emergency treatment or dial 9-1-1.
Stage 3: Gray hepatization
Red blood cells will disintegrate during this stage, giving the lungs a grayish color. However, immune cells remain, and symptoms will likely persist.Stage 4: Resolution
During the resolution phase, seniors may begin to feel better as immune cells rid their bodies of infection. However, they may develop a productive cough that helps to remove fluid from the lungs.
Normally you will start by asking about medical history and doing a physical exam, including listening to your lungs with a stethoscope to check for abnormal bubbling or crackling sounds that suggest pneumonia.
If pneumonia is suspected, the following tests are recommended:
- Blood tests. Blood tests are used to confirm an infection and to try to identify the type of organism causing the infection. However, precise identification isn't always possible.
- Chest X-ray. This helps your doctor diagnose pneumonia and determine the extent and location of the infection. However, it can't tell your doctor what kind of germ is causing the pneumonia.
- Pulse oximetry. This measures the oxygen level in your blood. Pneumonia can prevent your lungs from moving enough oxygen into your bloodstream.
- Sputum test. A sample of fluid from your lungs (sputum) is taken after a deep cough and analyzed to help pinpoint the cause of the infection.
Management of Pneumonia
Treatment for pneumonia involves curing the infection and preventing complications.
People who have community-acquired pneumonia usually can be treated at home with medication. Although most symptoms ease in a few days or weeks, the feeling of tiredness can persist for a month or more.
Specific treatments depend on the type and severity of your pneumonia, your age and your overall health. The options include:
- Antibiotics: These medicines are used to treat bacterial pneumonia. It may take time to identify the type of bacteria causing your pneumonia and to choose the best antibiotic to treat it. If your symptoms don't improve, your doctor may recommend a different antibiotic.
- Cough medicine: This medicine may be used to calm your cough so that you can rest. Because coughing helps loosen and move fluid from your lungs, it's a good idea not to eliminate your cough completely. In addition, you should know that very few studies have looked at whether over-the-counter cough medicines lessen coughing caused by pneumonia. If you want to try a cough suppressant, use the lowest dose that helps you rest.
- Fever reducers/pain relievers: You may take these as needed for fever and discomfort. These include drugs such as aspirin, ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others).
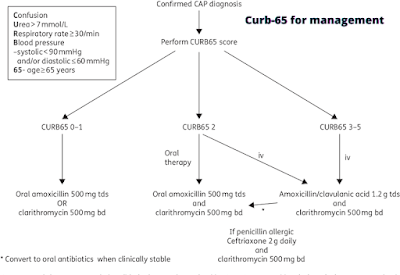
CURB-65 Management
Hospitalization
You may need to be hospitalized if:
- You are older than age 65
- You are confused about time, people or places
- Your kidney function has declined
- Your systolic blood pressure is below 90 millimeters of mercury (mm Hg) or your diastolic blood pressure is 60 mm Hg or below
- Your breathing is rapid (30 breaths or more a minute)
- You need breathing assistance
- Your temperature is below normal
- Your heart rate is below 50 or above 100
You may be admitted to the intensive care unit if you need to be placed on a breathing machine (ventilator) or if your symptoms are severe.
Children may be hospitalized if:
- They are younger than age 2 months
- They are lethargic or excessively sleepy
- They have trouble breathing
- They have low blood oxygen levels
- They appear dehydrated


No comments:
Post a Comment